MEDI-CAL

Here you will find:
- “What Counts as Income”
- “Frequently Asked Questions”
- “Sample Medi-Cal Letters”
Please review these sections below to help determine whether you are eligible for Medi-Cal or for a subsidy through Covered California.
**PLEASE NOTE: If you are married, you must file your taxes as
Married Filing Jointly to qualify for a subsidy. If you file as Married Filing Separately, you WILL NOT qualify for any subsidy amount.
What Counts as Income?
In order to determine how much financial help you can get, you will need to estimate your household income for the current year.
Include income from anyone you claim on your taxes.
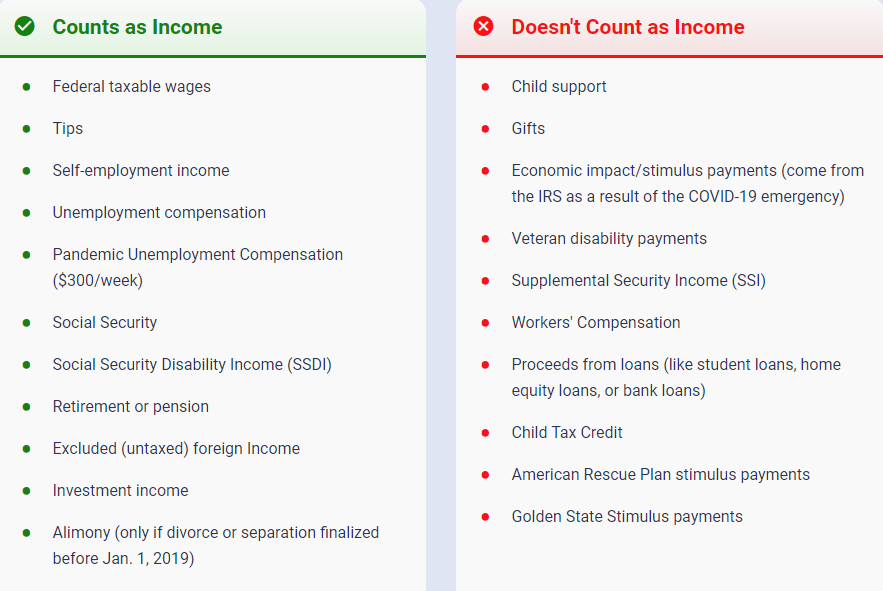
If you think your income may change in the future and aren’t sure how much costs are going to change, click on the Shop & Compare link below:
Shop & Compare Health Insurance Plans | Covered California™
**If your estimated income changes during the year,
please be sure to update your Covered California account accordingly.**
What Counts as Income instructions are current as of 04/08/2024.
Frequently Asked Questions
- Why was I sent to Medi-Cal?
In general, qualifying for Medi-Cal is based on income. Households earning less than 138% of the federal poverty level (FPL) will qualify and be routed to Medi-Cal. The size of your household affects the maximum amount to qualify. - I believe I was sent to Medi-Cal in error. How should I proceed?
If you received a letter saying you or your family member(s) are now on Medi-Cal, but you believe this is an error, you will need to update your income with the county. Call the contact number listed on the letter you received with your Case Number or Social Security number. See “What Counts As Income” above before you call. - Is it possible for the members of the same family to qualify for different coverage at the same time?
The Covered California application is a single application for multiple health coverage programs. Commonly, members of the same family or tax household are eligible for different programs.- For example, both parents could be eligible for tax credits through Covered California, while the children are eligible for Medi-Cal.
- This is because the eligibility rules for kids are different than those for adults.
- This is referred to as a “Mixed Household” – see example letter here.
- In these instances, you will be required to provide documentation to both the Medi-Cal and Covered California upon request to verify eligibility.
- Lack of providing requested information will result in a negative action that could negatively affect coverage for the entire household.
- For example, both parents could be eligible for tax credits through Covered California, while the children are eligible for Medi-Cal.
- How do I get released from Medi-Cal?
Contact your local county office. If the information you provided on your application has changed, you must report that change to your local county office. Call the office ahead of time for instructions on how to proceed.- County office contact information is available at http://www.dhcs.ca.gov/services/medi-cal/Pages/CountyOffices.aspx.
- When you get a social worker on the phone, tell them that you want to report a change to your Medi-Cal information (an income increase is generally what’s needed to be released).
- Ask specifically what documents you’ll need to provide and the best way to submit them. Take down the social worker’s name in case you have any questions or issues later.
- Gather documentation. You’ll have to provide documentation of the change when you report it. You’ll save time and prevent multiple trips if you get your proof together before you go to your local county office.
- You can find a list of acceptable documents on the www.benefitscal.com website. If you haven’t already, register for a free account on the website. Some counties allow you to upload the required documentation directly on their site.
- You can find a list of acceptable documents on the www.benefitscal.com website. If you haven’t already, register for a free account on the website. Some counties allow you to upload the required documentation directly on their site.
- How long does it take to be released from Medi-Cal?
It can normally take up to 45 days for the county to go through its general verification process and determine whether you qualify and/or route you back to Covered California. - If someone’s Medi-Cal coverage is canceled due to increased income or decreased household size, does that person qualify for special enrollment into Covered California?
Yes, losing health coverage such as Medi-Cal is considered a qualifying event that would trigger a Special Enrollment Period (SEP). - My Medi-Cal has been discontinued, and I am now able to enroll in Covered California during a Special Enrollment Period (SEP). How can I avoid a gap in my health coverage?
If your Medi-Cal will be or has been discontinued, to avoid a gap in your health coverage you should pick a Covered California plan before the date your Medi-Cal ends.- If you do not select a Covered California plan in the same month your Medi-Cal ends, you will not have health care coverage for at least a month.
- You must also pay your Covered California premium by the due date shown when you are billed to be covered.
- If your enrollment request is completed within 60 days of the qualifying life event date, the soonest your Covered California health plan can start will be the 1st of the month following your Covered California plan selection.
- If you wait more than 60 days after your Medi-Cal ends to pick a Covered California plan, you may not be able to enroll until Covered California’s next Open Enrollment Period.
- Can I decline Medi-Cal and enroll in a Covered California health plan and receive federal premium assistance?
Under federal law, if you are currently enrolled in or are eligible for Medi-Cal, you are ineligible to purchase subsidized coverage through Covered California.- If you are eligible for Medi-Cal, you can still purchase a health coverage plan through Covered California, but you cannot receive premium assistance to reduce its cost and will have to pay the full cost of the Covered California health care plan’s premium.
Sample Medi-Cal Letters
Below are examples of the types of letters you
may have received from Medi-Cal:
Example 1 (You’re Being Sent to Medi-Cal instead of Covered California):
This is an example of a letter typically received when you are being sent to Medi-Cal and your Covered California plan is being terminated.
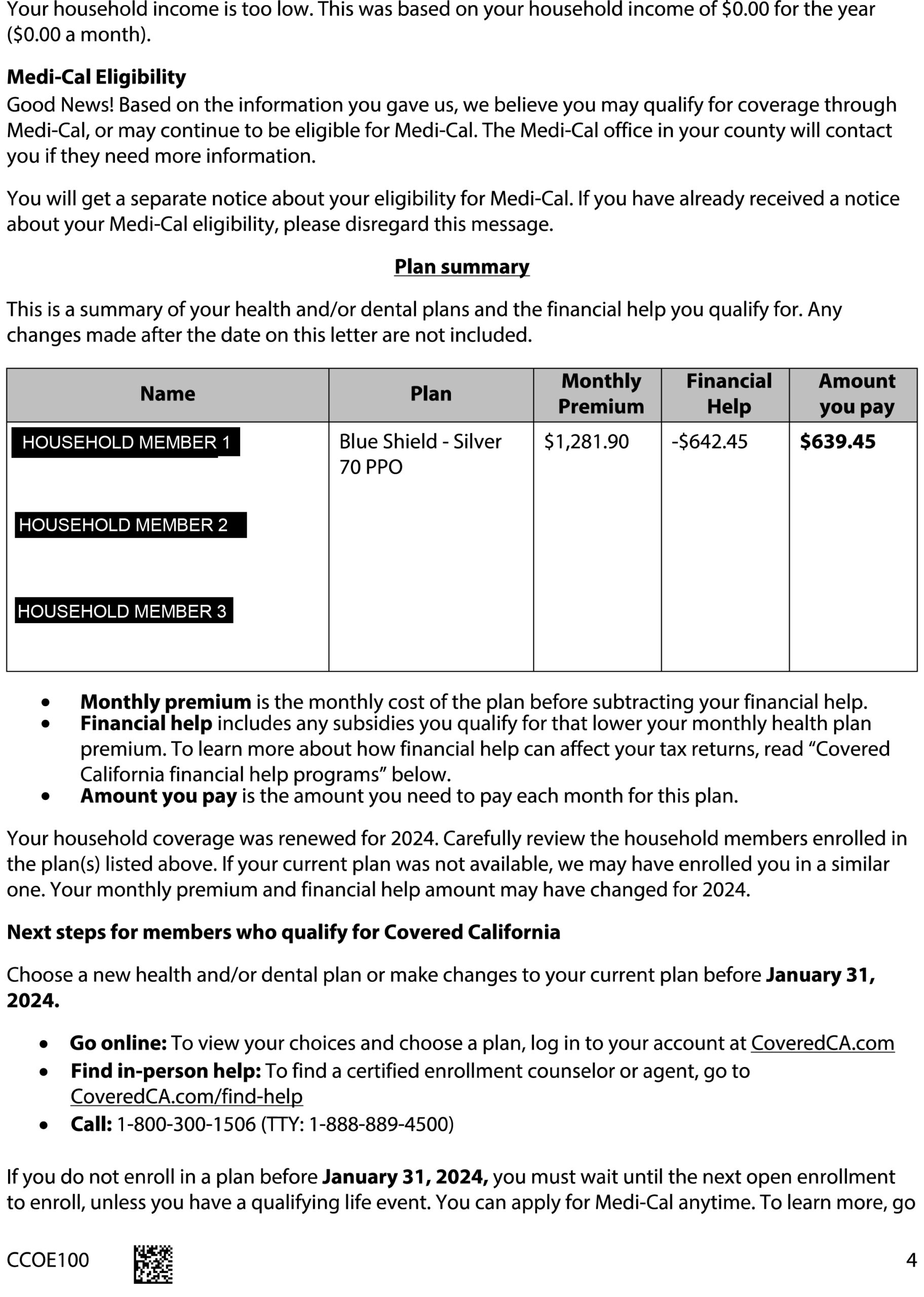
Example 2 (Carry-Forward to Medi-Cal in Review):
This is an example of what you will receive if your case is in Carry-Forward status. Carry-Forward status means your case has been sent to the county for review to determine whether you or household member(s) will be moved to Medi-Cal instead of Covered California. You can keep your current Covered California plan in the meantime, but it is often without premium assistance while the county verifies your eligibility.
Example 3 (Medi-Cal & Covered CA – Mixed Household):
Example 4 (Medi-Cal Approved or Denied by Member):
Example 5 (No Longer Qualify for Medi-Cal):